In 1978, the world’s governments came together and committed to the Alma Ata Declaration – a 20th century milestone in public health to protect and promote the health of all people. In the subsequent four decades, those called to action by the declaration have shown varied levels of commitment to its principles.
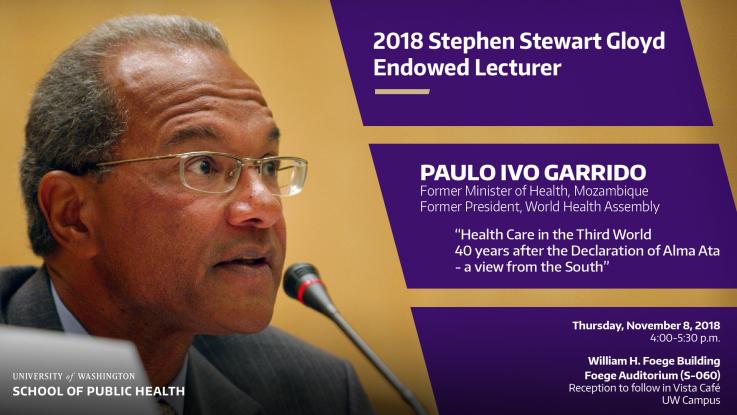
Paulo Ivo Garrido, former Minister of Health of Mozambique and president of the 59th World Health Assembly, played key roles in Alma Ata and its implementation. As this year’s Stephen Stewart Gloyd Endowed Lecturer, Dr. Garrido will share a unique perspective on the Alma-Ata Declaration of 1978, when Mozambique and other countries were creating their own pathways to primary health care. Ahead of the upcoming lecture, we sat down with Dr. Garrido to learn more about Alma Ata and what we as citizens can do to promote health care for the people by the people.
Please join Dr. Garrido for the Stephen Stewart Gloyd Lecture, 4-6:30 p.m., Thursday, Nov. 8, 2018 at Foege Auditorium (S-060). Preceding the Lecture is moderated panel discussion at 2:30 p.m. in the Foege Vista Café on the legacy of Alma Ata and celebrating the 40th anniversary of the Alma Ata Declaration.
What is the Alma Ata Declaration, and how are you involved in promoting the Primary Health Care – Alma Ata concept?
The Declaration of Alma Ata is a short document, a little over two pages, that was issued at the end of an international conference on primary health care that was held in September 1978 in the town of Alma Ata (now called Almaty), the capital of what is today the Republic of Kazakhstan. Besides defining the concept of Primary Health Care, the Declaration:
- Helped to entrench the idea that health is a human right.
- Noted that “the gross inequality in the health status of the people between developed and developing countries as well as within countries, is politically, socially and economically unacceptable.”
- Identified the mutual relationship between economic and social development and improving the health status of citizens. For the first time, economic and social determinants of health were clearly stated in a document of global significance.
- Established community participation as a pillar of primary health care. It is health care for the people and by the people.
The concept of primary health care evolved from failed experiences both in high- and low-income countries, in particular the failure of the Malaria Eradication Program and other vertical top-down approaches to health care.
I was involved in the definition of Mozambique’s National Health Policy, based on the Primary Health Care – Alma Ata concept. I was part of the team that, in the late seventies, wrote the book “Primary Health Care in Mozambique.” From 2005 to 2010, as Minister of Health of Mozambique, my main focus was on implementing the Primary Health Care – Alma Ata concept in my country. At that time one of our successes was the elimination of leprosy, certified by the WHO.
How is the Primary Health Care – Alma Ata concept different than the concept of universal health coverage?
The Primary Health Care – Alma Ata concept is a much broader concept than universal health coverage (UHC). Theoretically there are several ways to achieve UHC, but my experience as a medical doctor and as Minister of Health of Mozambique showed me that the best way is precisely through Primary Health Care – Alma Ata.
To what extent has the Alma Ata call for “Health for all by 2000” been achieved?
Unfortunately the Alma Ata call for “Health for all by 2000” has not been totally achieved in any country, although some countries (such as Cuba and some Nordic countries) are very advanced in that direction. Some of the facilitators were and still are the leadership of WHO and UNICEF and the political will of a few governments (Mozambique included). The main barriers were and still are the misunderstanding and distortion of the concept of Primary Health Care, the lack of political will by the many governments, the lack of funding, as well as incorrect health policies imposed by the donor community (especially the World Bank and the IMF) in low- and middle-income countries.
What have been some major achievements of Mozambique’s pathway toward primary health care since the 1970s?
The major achievements in Mozambique’s pathway toward primary health care were the introduction of free health care for all, the elimination of the fragmented and racist character of health services, the continuing extension of the health care network especially for rural areas and the priority to promote primary health care.
What are the main challenges?
The main challenges that remain today in Mozambique’s pathway to PHC are a tremendous shortage of health workers of all types and chronic under-financing of the health sector. Although there are a few exceptions, the actions of most NGOs and the donor community hinder the achievement by the government of Mozambique of Primary Health Care as defined in the Declaration of Alma Ata.
To give you two examples: the macroeconomic policies imposed on Mozambique by the World Bank and the IMF involve restrictions on the government’s ability to hire human resources for health. This means that – despite the tremendous shortage of human resources for health – at least over the last 15 years the government of Mozambique has not been able to hire all of the few doctors, nurses, pharmacists and other health workers trained in the country. Another example is that while the main sector of Mozambique’s health system is the public sector (National Health Service), which covers more than 80% of the population, most donors have chosen to channel much of their funds to NGOs implementing vertical, top down activities rather than to the National Health Service.
How might high-income country donors help address these challenges?
High-income country donors can help address these challenges by altering their primary health care policies, funding and/or programs to be more helpful to low-income countries through:
- Providing a larger proportion of aid as long-term National Health Service budget support.
- Not promoting inappropriate approaches in the name of UHC, especially vertical programs.
- Supporting, in particular, governments that make equity and universality explicit priorities from the outset.
- Taking action on tax avoidance and tax evasion that denies low-income countries much-needed revenue for universal public services.
- Honoring their commitments to provide at least 0.7 per cent of Gross National Income as Official Development Assistance, and improve aid effectiveness for health.
What can we do as citizens to further the ambitions of Primary Health Care – Alma Ata?
As responsible citizens from high-income countries you can firstly understand the Declaration of Alma Ata, which clearly states that “every citizen has the right and the duty to participate individually and collectively in the planning and implementation of their healthcare,” and stop passively accepting what governments and doctors say is best for your health care without consulting you.I hope all citizens use their power to put pressure on their governments to take action in ways described in the question above.